India Hits a Milestone: ISRO Launches Its Heaviest Communication Satellite Yet, CMS-03
Lupus Disease : Symptoms, Causes, Diagnosis, and Treatment – A Complete Guide

Lupus Disease
Lupus Disease is a complex and often misunderstood chronic autoimmune disease that can affect virtually any part of the body. By raising awareness and providing clear, accurate information, this blog aims to help readers understand what lupus is, its symptoms, causes, diagnosis, and treatment options. Whether you’re newly diagnosed, supporting a loved one, or simply curious, this guide offers a detailed yet accessible overview of lupus.
What is Lupus Disease ?
Lupus Disease is an autoimmune condition where the immune system, which typically protects the body from infections, mistakenly attacks its own healthy tissues. This leads to inflammation and damage in various organs and systems, such as the skin, joints, kidneys, heart, lungs, and brain. The most common form of lupus is systemic lupus erythematosus (SLE), but other types include:
- Cutaneous lupus: Primarily affects the skin, causing rashes or sores.
- Drug-induced lupus: Triggered by certain medications, with symptoms that often resolve after discontinuing the drug.
- Neonatal lupus: A rare condition affecting newborns of mothers with lupus, typically involving skin rashes or heart issues.
Lupus is not contagious, and while it can range from mild to life-threatening, proper management can significantly improve quality of life.

Who is Affected by Lupus?
Lupus affects approximately 1.5 million people in the United States and 5 million worldwide. It disproportionately impacts certain groups:
- Gender: Women are nine times more likely to develop lupus than men, likely due to hormonal influences.
- Age: Most commonly diagnosed between ages 15 and 45, though it can occur at any age.
- Ethnicity: Higher prevalence among African American, Hispanic, Asian, and Native American populations compared to Caucasian individuals.
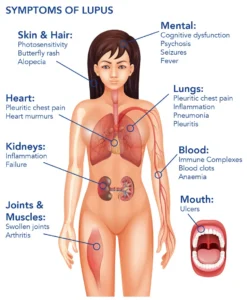
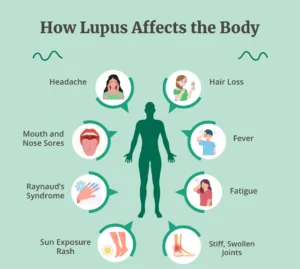
Symptoms of Lupus Disease
Lupus is often called the “disease of a thousand faces” because its symptoms vary widely and can mimic other conditions. Symptoms may come and go in episodes called flares, followed by periods of remission. Common symptoms include:
- Fatigue: Persistent, overwhelming tiredness that doesn’t improve with rest.
- Joint Pain and Swelling: Stiffness or pain in joints, especially in the hands, wrists, and knees.
- Skin Rashes: A hallmark is the butterfly-shaped rash across the cheeks and nose, often triggered by sun exposure. Other rashes or sores may appear elsewhere.
- Fever: Unexplained low-grade fevers during flares.
- Photosensitivity: Sensitivity to sunlight, which can worsen rashes or trigger flares.
- Hair Loss: Thinning hair or patchy hair loss, often temporary.
- Mouth or Nasal Sores: Painless ulcers inside the mouth or nose.
- Organ Involvement: Lupus can affect the kidneys (lupus nephritis), heart, lungs, or brain, leading to symptoms like chest pain, shortness of breath, or neurological issues (e.g., seizures, memory problems).
Because symptoms vary, lupus can be challenging to recognize, often leading to delayed diagnosis.
What Causes Lupus Disease?
The exact cause of lupus remains unknown, but it’s believed to result from a combination of factors:
- Genetics: A family history of lupus or other autoimmune diseases increases risk, though no single “lupus gene” exists.
- Environmental Triggers: Exposure to ultraviolet (UV) light, certain infections (e.g., Epstein-Barr virus), smoking, or specific medications (e.g., hydralazine, procainamide) can trigger or worsen lupus.
- Hormonal Factors: Estrogen may play a role, explaining the higher prevalence in women, especially during reproductive years or pregnancy.
- Immune System Dysregulation: Abnormal immune responses cause the body to produce autoantibodies, like antinuclear antibodies (ANA), that attack healthy tissues.
Diagnosing Lupus Disease
Diagnosing lupus is complex because no single test confirms it. Doctors rely on a combination of:
- Medical History and Symptoms: Evaluating the patient’s symptoms and family history.
- Physical Examination: Checking for rashes, joint swelling, or other signs.
- Blood Tests:
- Antinuclear Antibody (ANA) Test: A positive ANA test is common in lupus but not specific to it.
- Tests for other autoantibodies (e.g., anti-dsDNA, anti-Smith) or complement levels (C3, C4).
- Urine Tests: To detect kidney involvement, such as protein or blood in the urine.
- Biopsies: In some cases, a kidney or skin biopsy confirms lupus-related damage.
The American College of Rheumatology provides classification criteria, requiring at least 4 of 11 specific signs or symptoms (e.g., butterfly rash, photosensitivity, kidney issues) for a formal SLE diagnosis.
Treatment and Management
While there’s no cure for lupus, treatments aim to control symptoms, prevent flares, and minimize organ damage. Treatment plans are tailored to the individual and may include:
- Medications:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Reduce joint pain and inflammation.
- Corticosteroids (e.g., prednisone): Control severe inflammation but used cautiously due to side effects.
- Antimalarials (e.g., hydroxychloroquine): Reduce flares and improve skin and joint symptoms.
- Immunosuppressants (e.g., methotrexate, azathioprine): Suppress the overactive immune system for severe cases.
- Biologics (e.g., belimumab): Target specific immune pathways.
- Lifestyle Changes:
- Sun Protection: Wear sunscreen, hats, and protective clothing to avoid UV-triggered flares.
- Healthy Diet: Focus on anti-inflammatory foods like fruits, vegetables, and omega-3-rich fish.
- Exercise: Low-impact activities like walking or yoga to maintain joint mobility and reduce fatigue.
- Stress Management: Techniques like meditation or therapy to minimize stress-induced flares.
- Regular Monitoring: Frequent check-ups to track disease activity and organ function.
Complications of Lupus Disease
If not properly managed, lupus can lead to serious complications, including:
- Lupus Nephritis: Kidney inflammation, which can progress to kidney failure if untreated.
- Cardiovascular Issues: Increased risk of heart disease, stroke, or blood clots.
- Lung Problems: Pleurisy (inflammation of the lung lining) or pulmonary hypertension.
- Neurological Effects: Seizures, memory issues, or mood disorders in severe cases.
Early diagnosis and consistent treatment significantly reduce the risk of complications.
Living with Lupus Disease
A lupus diagnosis can feel overwhelming, but many people lead fulfilling lives with proper care. Key tips for managing lupus include:
- Build a Support System: Connect with healthcare providers, family, friends, or lupus support groups.
- Stay Informed: Learn about the condition to advocate for your needs.
- Track Symptoms: Keep a journal to identify triggers and share with your doctor.
- Prioritize Self-Care: Balance rest and activity, and address mental health needs.
Raising Awareness
Lupus awareness is critical because its unpredictable nature and varied symptoms often lead to misdiagnosis or delayed treatment. Organizations like the Lupus Foundation of America provide resources, support, and advocacy for patients and families. By sharing knowledge, we can reduce stigma and improve outcomes for those affected.
Also Read This : 90s Retro Look Prompt : How to Create a Stunning 90s Retro Look with AI, Step-by-Step Guide
Lupus is a challenging but manageable condition. With advances in treatment and growing awareness, people with lupus can live healthier, more active lives. If you suspect you or a loved one may have lupus, consult a healthcare provider for evaluation and guidance. Stay proactive, stay informed, and know that you’re not alone in navigating this journey.


